Sexually transmitted diseases (STDs) are passed from one person to another through intimate physical
contact – such as heavy petting..
What are STDs?
Sexually transmitted diseases (STDs) are passed from one person to another through intimate physical contact – such as heavy petting – and from sexual activity including vaginal, oral, and anal sex. STDs are very common. In fact, CDC estimates 20 million new infections occur every year in the United States. STDs can mostly be prevented by not having sex. If you do have sex, you can lower your risk by using condoms and being in a sexual relationship with a partner who does not have an STD. STDs do not always cause symptoms, so it is possible to have an infection and not know it. That is why it is important to
get tested if you are having sex. If you are diagnosed with an STD, know that all can be treated with medicine and some can be cured entirely.
There are dozens of STDs. Some STDs, such as syphilis, gonorrhea, and chlamydia, are spread mainly by sexual contact. Other diseases, including
Zika and
Ebola,
can be spread sexually but are more often spread through ways other than sex.
The diseases, conditions, and infections below are listed in alphabetical order.

Any woman can get bacterial vaginosis. Having bacterial vaginosis can increase your chance of getting an STD.

Chlamydia is a common sexually transmitted disease (STD) that can be easily cured. If left untreated, chlamydia can make it difficult for a woman to get pregnant.

Anyone who is sexually active can get gonorrhea. Gonorrhea can cause very serious complications when not treated, but can be cured with the right medication.

Viral hepatitis is the leading cause of liver cancer and the most common reason for liver transplantation.

Genital herpes is a common STD, and most people with genital herpes infection do not know they have it.

People who have STDs are more likely to get HIV, when compared to people who do not have STDs.

Human papillomavirus (HPV) is the most common sexually transmitted infection in the United States. Some health effects caused by HPV can be prevented with vaccines.

Pelvic Inflammatory Disease (PID) can lead to serious consequences including infertility.

Chlamydia and gonorrhea are preventable causes of pelvic inflammatory disease (PID) and infertility.

For a healthier baby, ask your doctor about STD testing.

Syphilis is a sexually transmitted disease (STD) that can have very serious complications when left untreated, but it is simple to cure with the right treatment.

Most people who have trichomoniasis do not have any symptoms.

Chancroid, scabies, and more.
STDs & Infertility
Chlamydia and gonorrhea are important preventable causes of pelvic inflammatory disease (PID) and infertility. Untreated, about 10-15% of women with chlamydia will develop PID. Chlamydia can also cause fallopian tube infection without any symptoms. PID and “silent” infection in the upper genital tract may cause permanent damage to the fallopian tubes, uterus, and surrounding tissues, which can lead to infertility.
- An estimated 2.86 million cases of chlamydia and 820,000 cases of gonorrhea occur annually in the United States.*
- Most women infected with chlamydia or gonorrhea have no symptoms.
CDC recommends annual chlamydia and gonorrhea screening of all sexually active women younger than 25 years, as well as older women with risk factors such as new or multiple sex partners, or a sex partner who has a sexually transmitted infection.
* Chlamydia and gonorrhea are the first and second most commonly reported notifiable disease in the United States. In 2017, a total of 1,708,569 chlamydial infections and 555,608 cases of gonorrhea were reported to CDC from 50 states and the District of Columbia. The number of reported cases is lower than the estimated total number because infected people are often unaware of, and do not seek treatment for, their infections and because screening for chlamydia is still not routine in many clinical settings.
STD Risk and Oral Sex - CDC Fact Sheet
Fast Facts
- Many sexually transmitted diseases (STDs) can be spread through oral sex.
- Using a condom, dental dam or other barrier method each and every time you have oral sex can reduce the risk of giving or getting an STD.
- Although oral sex may carry a lower risk for spreading HIV than other forms of sex, repeated unprotected exposures may increase risk of transmission.
What is Oral Sex?
Oral sex involves using the mouth, lips, or tongue to stimulate the penis (fellatio), vagina (cunnilingus), or anus (anilingus) of a sex partner. The penis and testicles and the vagina and area around the vagina are also called the genitals or genital area.
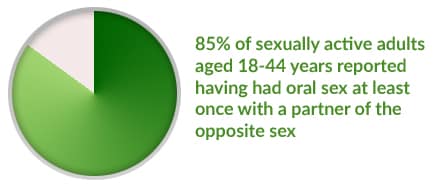
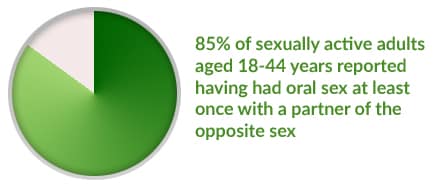
How Common is Oral Sex?
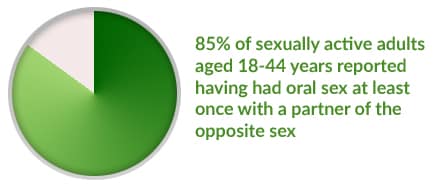
Oral sex is commonly practiced by sexually active adults. Oral sex can happen between heterosexual (straight) and same-sex (gay or lesbian) couples. More than 85% of sexually active adults aged 18-44 years reported having had oral sex at least once with a partner of the opposite sex. A separate survey conducted during 2007-2010 found that 33% of teenage girls and boys aged 15-17 years reported having had oral sex with a partner of the opposite sex.
Can STDs Be Spread During Oral Sex?
Many STDs, as well as other infections, can be spread through oral sex. Anyone exposed to an infected partner can get an STD in the mouth, throat, genitals, or rectum. The risk of getting an STD from oral sex, or spreading an STD to others through oral sex, depends on a number of things, including
- The particular STD.
- The sex acts practiced.
- How common the STD is in the population to which the sex partners belong.
- The number of specific sex acts performed.
In general:
- It may be possible to get some STDs in the mouth or throat from giving oral sex to a partner with a genital or anal/rectal infection, particularly from giving oral sex to a partner with an infected penis.
- It also may be possible to get certain STDs on the penis (and possibly the vagina, anus or rectum) from getting oral sex from a partner with a mouth or throat infection.
- It’s possible to have an STD in more than one area at the same time, for example in the throat and the genitals.
- Several STDs that may be transmitted by oral sex can then spread throughout the body of an infected person.
- STDs can be spread to a sex partner even when the infected partner has no signs or symptoms. If you are infected with an STD, you might not know it because many STDs may have no symptoms.
Which STDs Can Be Passed On from Oral Sex?
 Chlamydia
Chlamydia
(Chlamydia trachomatis)
Risk of infection from oral sex:
- Giving oral sex to a man with an infected penis can result in getting chlamydia in the throat.
- Giving oral sex to a woman with an infected vagina or urinary tract may result in getting chlamydia in the throat.*
- Giving oral sex to a man or woman with an infected rectum might result in getting chlamydia in the throat.*
- Getting oral sex on the penis from a partner with chlamydia in the throat can result in getting chlamydia of the penis.
- Getting oral sex on the vagina from a partner with chlamydia in the throat might result in getting chlamydia of the vagina or urinary tract.*
- Getting oral sex on the anus from a partner with chlamydia in the throat might result in getting chlamydia in the rectum.*
* Statements followed by an asterisk (*) have not been well studied.
Areas of initial infection:
- Throat
- Genitals
- Urinary tract
- Rectum
Initial signs and symptoms of infection:
- Most chlamydia infections in the throat have no symptoms. When symptoms are present, they can include a sore throat.
- Many genital, urinary tract, or rectal chlamydia infections have no symptoms. When symptoms are present, they can include:
- Discharge from vagina or penis (discharge from the vagina may be bloody).
- Burning feeling when urinating.
- Painful or swollen testicles.
- Rectal pain or discharge
Treatment:
- Chlamydia can be cured with the right medicine.
- The sex partners of a person with chlamydia should also be tested for infection. Those who are diagnosed with chlamydia should not have sex until they and their sex partners have completed treatment.
If left untreated, throat infections:
- Can be spread to uninfected sex partners, particularly by performing oral sex on a male partner’s penis.
If left untreated, genital, urinary and/or rectal infections:
- Can be spread to uninfected sex partners.
- In women:
- In pregnant women:
- Might result in premature birth or low birth weight in babies.
- Can be spread to the baby during delivery, and can cause chlamydia infection in the eyes or infection of the respiratory tract that can develop into pneumonia.
- In men:
- Can cause epididymitis, a painful condition of the ducts attached to the testicles that may lead to ductal scarring.
- In both men and women:
- May increase risk of getting HIV infection.
- Might increase risk of spreading HIV to sex partners.
- May cause a reaction (reactive arthritis) throughout the body that can lead to arthritis (joint pain), conjunctivitis (pink eye), and/or a rash on the soles of the feet or elsewhere.
In addition to the STDs above, other infections such as
hepatitis A virus,
Shigella and intestinal parasites (
amebiasis) can be spread through giving oral sex on the anus.
Is Oral Sex Safer than Vaginal or Anal Sex?

- Many STDs can be spread through oral sex. However, it is difficult to compare the exact risks of getting specific STDs from specific types of sexual activity. This is partly because most people who have oral sex also have vaginal or anal sex. Also, few studies have looked at the risks of getting STDs other than HIV from giving oral sex on the vagina or anus, compared to giving oral sex on the penis.
- Studies have shown that the risk of getting HIV from having oral sex with an infected partner (either giving or getting oral sex) is much lower than the risk of getting HIV from anal or vaginal sex with an infected partner. This may not be true for other STDs – in one study of gay men with syphilis, 1 out of 5 reported having only oral sex.
- Getting HIV from oral sex may be less likely than vaginal or anal sex, but it still carries risk. If you are having oral sex you should still protect yourself. Repeated unprotected oral sex exposure to HIV may represent a considerable risk for spread of HIV, as well as other STDs for which the risk of spread through oral sex has not been as well studied.
- It is possible that getting certain STDs, such as chlamydia or gonorrhea, in the throat may not pose as great a threat to an infected person’s health as getting an STD in the genital area or rectum. Having these infections in the throat might increase the risk of getting HIV. Having gonorrhea in the throat also may lead to spread of the disease throughout the body. In addition:
- Having infections of chlamydia and gonorrhea in the throat may make it easier to spread these infections to others through oral sex. This is especially important for gonorrhea, since throat infections are harder to treat than urinary, genital or rectal infections.
- Infections from certain STDs, such as syphilis and HIV, spread throughout the body. Therefore, infections that are acquired in the throat may lead to the same health problems as infections acquired in the genitals or rectum.
- Mouth and throat infections by certain types of HPV may develop into oral or neck cancer.
What May Increase the Chances of Giving or Getting an STD through Oral Sex?
It is possible that certain factors may increase a person’s chances of getting HIV or other STDs during oral sex if exposed to an infected partner, such as:
- Having poor oral health which can include tooth decay, gum disease or bleeding gums, and oral cancer.
- Having sores in the mouth or on the genitals.
- Being exposed to the “pre-cum” or “cum” (also known as pre-ejaculate or ejaculate) of an infected partner.
However, no scientific studies have been done to show whether or not these factors actually do increase the risk of getting HIV or STDs from oral sex.
What Can You Do to Prevent STD Transmission During Oral Sex?
You can lower your chances of giving or getting STDs during oral sex by using a condom, dental dam or other barrier method each and every time you have oral sex.
- For oral sex on the penis:
- Cover the penis with a non-lubricated latex condom.
- Use plastic (polyurethane) condoms if you or your partner is allergic to latex.
- For oral sex on the vagina or anus:
- Use a dental dam.
- Cut open a condom to make a square, and put it between the mouth and the partner’s vagina or anus.
The only way to avoid STDs is to not have vaginal, anal, or oral sex.
If you are sexually active, you can do the following things to lower your chances of getting an STD:
- Being in a long-term mutually monogamous relationship with a partner who is not infected with an STD (e.g., a partner who has been tested and has negative STD test results).
- Using latex condoms the right way every time you have sex.
It’s important to remember that many infected individuals may be unaware of their infection because STDs often have no symptoms and are unrecognized.
If you are sexually active, you should get tested regularly for STDs and HIV and talk to your partner(s) about STDs. If you think you might have an STD, stop having sex and visit your doctor or clinic to get tested. There are free and low-cost options for testing in your area. It is important that you talk openly with your health care provider about any activities that might put you at risk for an STD, including oral sex.
How You Can Prevent Sexually Transmitted Diseases
Abstinence; The most reliable way to avoid infection is to not have sex (i.e., anal, vaginal or oral).
Vaccination:Vaccines are safe, effective, and recommended ways to prevent hepatitis B and HPV. HPV vaccinesfor males and females can protect against some of the most common types of HPV. It is best to get all three doses (shots) before becoming sexually active.
However, HPV vaccines are recommended for all teen girls and women through age 26 and all teen boys and men through age 21, who did not get all three doses of the vaccine when they were younger. You should also get vaccinated for hepatitis B if you were not vaccinated when you were younger.
Reduce Number of Sex Partners: Reducing your number of sex partners can decrease your risk for STDs. It is still important that you and your partner get tested, and that you share your test results with one another.
Mutual Monogamy: Mutual monogamy means that you agree to be sexually active with only one person, who has agreed to be sexually active only with you. Being in a long-term mutually monogamous relationship with an uninfected partner is one of the most reliable ways to avoid STDs. But you must both be certain you are not infected with STDs. It is important to have an open and honest conversation with your partner.
Use Condoms: Correct and consistent use of the male latex condom is highly effective in reducing STD transmission. Use a condom every time you have anal, vaginal, or oral sex.
If you have latex allergies, synthetic non-latex condoms can be used. But it is important to note that these condoms have higher breakage rates than latex condoms. Natural membrane condoms are not recommended for STD prevention.
“The Lowdown” Infographic: “The Lowdown on how to Prevent STDs” infographic.
Expedited Partner Therapy:
Expedited Partner Therapy (EPT) is the clinical practice of treating the sex partners of patients diagnosed with chlamydia or gonorrhea by providing prescriptions or medications to the patient to take to his/her partner without the health care provider first examining the partner.
Effective clinical management of patients with treatable sexually transmitted diseases (STDs) requires treatment of the patients’ current sex partners to prevent reinfection and curtail further transmission. The standard approach to partner treatment has included clinical evaluation in a health care setting, with partner notification accomplished by the index patient, by the provider or an agent of the provider, or a combination of these methods. Provider-assisted referral is considered the optimal strategy for partner treatment, but is not available to most patients with gonorrhea or chlamydial infection because of resource limitations. The usual alternative is to advise patients to refer their partners for treatment.
CDC has concluded that EPT is a useful option to facilitate partner management, particularly for treatment of male partners of women with chlamydial infection or gonorrhea. Although ongoing evaluation will be needed to define when and how EPT can be best utilized, the evidence indicates that EPT should be available to clinicians as an option for partner treatment. EPT represents an additional strategy for partner management that does not replace other strategies such as provider-assisted referral, when available.






























Comments
Post a Comment